Polyuria-polydipsia Syndrome
Improved differential diagnosis in your endocrine practice
The challenge in the diagnosis of the polyuria-polydipsia syndrome is differentiating between cases of primary polydipsia and diabetes insipidus.
A single Copeptin measurement can immediately distinguish central diabetes insipidus from nephrogenic diabetes insipidus. As a consequence, Copeptin measurement reduces the burden of the water deprivation test for the majority of patients and improves patient management within the clinic. Ref-1
Smart Copeptin testing
- Reliable results
- Reduced costs (fewer measurements, less personnel and time)
- Simplified lab workflow
- Optimized patient management
Without Copeptin the diagnostic method of choice would be direct vasopressin determination, but the molecular characteristics of vasopressin make such measurement very complex and error-prone, hence unreliable. Consequently, “direct vasopressin testing” has not been established as a diagnostic routine.
Further links on the advantages of Copeptin measurement
B·R·A·H·M·S Copeptin proAVP in your clinical routine for the differential diagnosis of polyuria-polydipsia syndrome
Polyuria-polydipsia syndrome (suspected diabetes insipidus)
- Excessive fluid intake and excessive urine volume
- Urine osmolality low, serum osmolality high
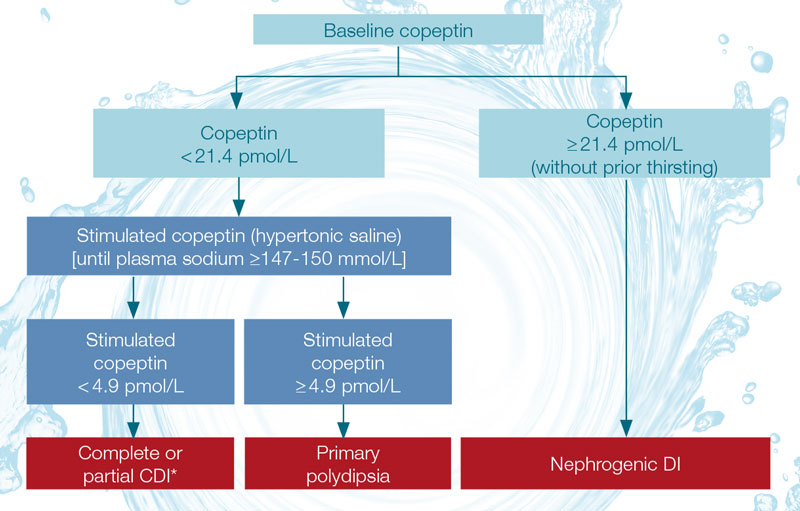 A diagnostic workflow for the differential diagnosis of polyuria-polydipsia syndrome, modified from Christ-Crain M et al. Ref-2
A diagnostic workflow for the differential diagnosis of polyuria-polydipsia syndrome, modified from Christ-Crain M et al. Ref-2
* CDI (Central Diabetes Insipidus), Nephrogenic DI (Nephrogenic Diabetes Insipidus)
References Polyuria-polydipsia syndrome
Ref-1: Timper K, Fenske W, et al. Diagnostic Accuracy of Copeptin in the Differential Diagnosis of the Polyuria-polydipsia Syndrome: A Prospective Multicenter Study. J Clin Endocrinol Metab, June 2015, 100(6):2268–22
Ref-2: Christ-Crain M et al., Nat Rev Endocrinol. 2016;12(3):168-76
