Pre-eclampsia Diagnosis and Prognosis
Improved pre-eclampsia diagnosis and prediction of adverse outcome after 20 weeks' gestation
- Pre-eclampsia is a life-threatening pregnancy related disorder which affects about 2-3% of pregnancies
- New onset of hypertension and/or proteinuria after 20 weeks of gestation are the first clinical signs and symptoms
- About 20% of the affected pregnancies are complicated by additional symptoms such as abdominal pain, haemorrhage, placental abruption or severe HELLP-syndrome (Hemolysis, Elevated Liver enzymes, Low Platelets)
- Eclampsia is the final stage of the disease, associated with tonic-clonic seizures and deathRef-1-2
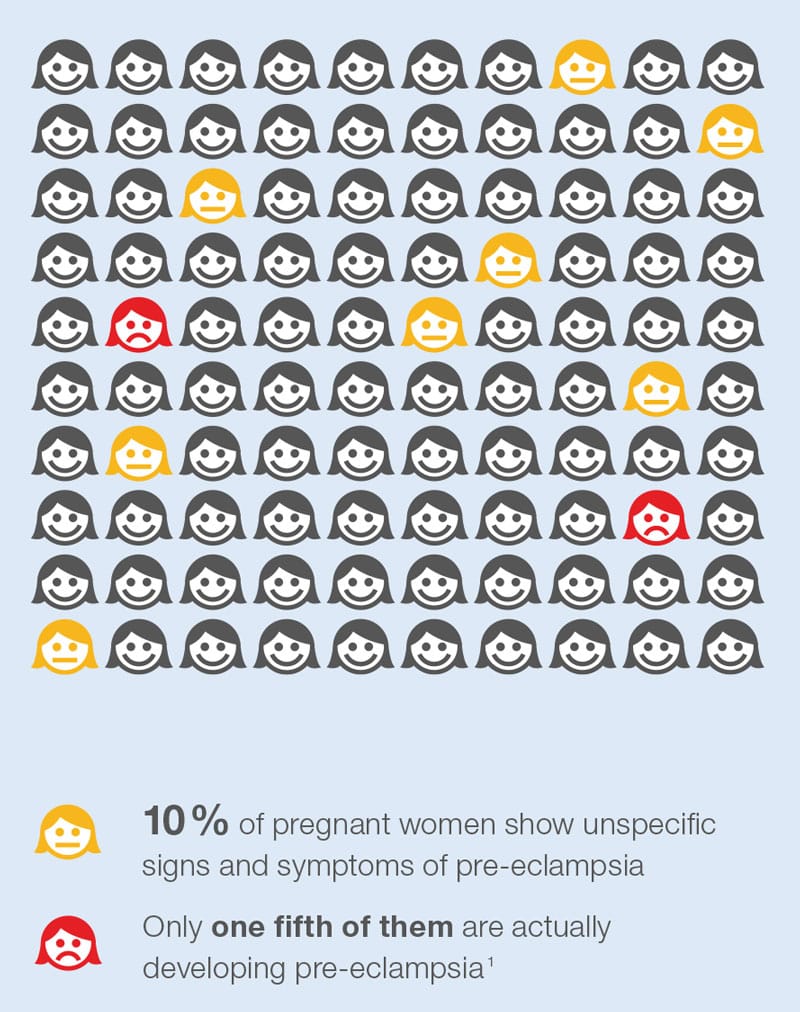
The first clinical signs of pre-eclampsia such as new onset of hypertension start to show in mid pregnancy, with about 10% of all pregnant women experiencing signs and symptoms of pre-eclampsia after 20 weeks’ gestation. Only one fifth of them will actually develop the diseaseRef-3.
The routine assessment to diagnose pre-eclampsia is measuring blood pressure and proteinuria, but these measurements offer only a limited sensitivity and specificity in predicting pre-eclampsia in symptomatic womenRef-4-5. This diagnostic standard can be significantly improved by using the serum biomarkers sFlt-1 and PlGF in addition to clinical routine procedures. The sFlt-1/PlGF ratio is a useful tool as an aid to:
- Confirm the diagnosis of pre-eclampsiaRef-6-9
- Differentiate between pre-eclampsia and other hypertensive pregnancy-related disordersRef-10-11
- Better prognose the development of an adverse outcome in pre-eclamptic womenRef-11-12
The high sensitivity assays Thermo Scientific B·R·A·H·M·S PlGF plus KRYPTOR and B·R·A·H·M·S sFlt-1 KRYPTOR can reliably detect PlGF and sFlt-1 in maternal serum to support an improved diagnosis and prognosis of pre-eclampsia after 20 weeks of gestation.
Watch expert opinion video
Clinical implementation of the sFlt-1/PlGF ratio to improve patient management
Prof. Stefan Verlohren, Department of Obstetrics, Charité Universitätsmedizin, Berlin, Germany
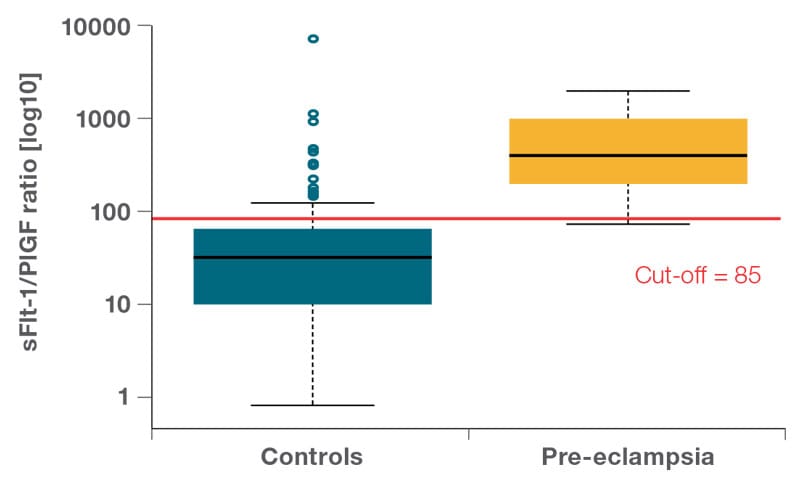
Improved pre-eclampsia diagnosis with sFlt-1/PlGF ratio
Women with hypertension due to pre-eclampsia have a significantly higher sFlt-1/PlGF ratio than women with any other form of hypertensive disorder.
At a cut-off of 85 for the sFlt-1/PlGF ratio, the sensitivity and specificity for diagnosing pre-eclampsia are 95% and 84%, respectively.
Benefits of the sFlt-1/PlGF ratio in diagnosing pre-eclampsia
- Significantly higher sensitivity and specificity in diagnosing pre-eclampsia than measuring blood pressure and proteinuriaRef-6
- Clearly differentiating between pre-eclampsia and other forms of hypertensive disordersRef-10
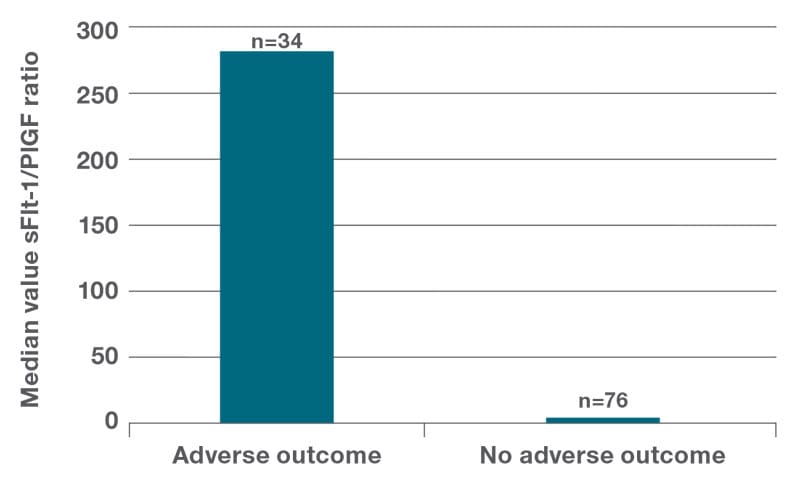
Short-term prognosis with sFlt-1/PlGF ratio in pre-eclamptic women
Women with any subsequent adverse outcome due to pre-eclampsia have a significantly higher sFlt-1/PlGF ratio than women with no complicationsRef-11-12.
Benefits of the sFlt-1/PlGF ratio as a predictor for adverse outcome
- Improved preparation time for delivery if neededRef-11-12
- Improved outbalancing of maternal risk vs fetal prematurityRef-11-12
Further links on pre-eclampia diagnosis
- Download our brochure on improved pre-eclampsia diagnosis after 20 weeks’ gestation.
- Download our literature review on improved pre-eclampsia diagnosis after 20 weeks’ gestation.
- Download our fact sheet on improved pre-eclampsia diagnosis after 20 weeks’ gestation.
- Find here a 10 minutes animation about pre-eclampsia management throughout pregnancy.
- Find here all our prenatal screening brochures, product sheets and other informational material.
References
Ref-1: L. Ghulmiyyah and B. Sibai, “Maternal Mortality From Preeclampsia/Eclampsia” Semin. Perinatol., vol. 36, no. 1, pp. 56–59, 2012.
Ref-2: C. E. Powe, R. J. Levine, and S. A. Karumanchi, “Preeclampsia, a disease of the maternal endothelium: The role of antiangiogenic factors and implications for later cardiovascular disease” Circulation, vol. 123, no. 24, pp. 2856–2869, 2011.
Ref-3: F. Milne et al., “Assessing the onset of pre-eclampsia in the hospital day unit: summary of the pre-eclampsia guideline (PRECOG II).” BMJ, vol. 339, no. 7721, p. b3129, Sep. 2009.
Ref-4: S. Verlohren, H. Stepan, and R. Dechend, “Angiogenic growth factors in the diagnosis and prediction of pre-eclampsia.” Clin. Sci. (Lond)., vol. 122, no. 2, pp. 43–52, Jan. 2012.
Ref-5: J. Zhang, M. A. Klebanoff, and J. M. Roberts, “Prediction of adverse outcomes by common definitions of hypertension in pregnancy.” Obstet. Gynecol., vol. 97, no. 2, pp. 261–7, Feb. 2001.
Ref-6: H. Hagmann, R. Thadhani, T. Benzing, S. A. Karumanchi, and H. Stepan, “The promise of angiogenic markers for the early diagnosis and prediction of preeclampsia.” Clin. Chem., vol. 58, no. 5, pp. 837–45, May 2012.
Ref-7: S. Verlohren et al., “An automated method for the determination of the sFlt-1/PIGF ratio in the assessment of preeclampsia.” Am. J. Obstet. Gynecol., vol. 202, no. 2, p. 161.e1-161.e11, Feb. 2010.
Ref-8: L. B. Andersen et al., “Diagnosis of preeclampsia with soluble Fms-like tyrosine kinase 1/placental growth factor ratio: an inter-assay comparison.” J. Am. Soc. Hypertens., vol. 9, no. 2, pp. 86–96, Feb. 2015.
Ref-9: J. van Helden and R. Weiskirchen, “Analytical evaluation of the novel soluble fms-like tyrosine kinase 1 and placental growth factor assays for the diagnosis of preeclampsia.” Clin. Biochem., vol. 48, no. 16–17, pp. 1113–9, Nov. 2015.
Ref-10: S. Verlohren et al., “The sFlt-1/PlGF ratio in different types of hypertensive pregnancy disorders and its prognostic potential in preeclamptic patients.” Am. J. Obstet. Gynecol., vol. 206, no. 1, p. 58.e1-8, Jan. 2012.
Ref-11: S. Rana et al., “Angiogenic factors and the risk of adverse outcomes in women with suspected preeclampsia.” Circulation, vol. 125, no. 7, pp. 911–9, Feb. 2012.
Ref-12: S. Salahuddin, J. B. Wenger, D. Zhang, R. Thadhani, S. A. Karumanchi, and S. Rana, “KRYPTOR-automated angiogenic factor assays and risk of preeclampsia-related adverse outcomes.” Hypertens. pregnancy, vol. 35, no. 3, pp. 330–45, Aug. 2016.